


Slit-lamp exam showed an inferior corneal thinning in both eyes, accentuated in the right eye. Case reportĪ 30-year-old female patient was referred to Hospital do Servidor Público Estadual - São Paulo in 1996 complaining of slowly and bilateral decreasing of visual acuity, worse in the right eye. This technique made it possible in this case to postpone the corneal transplant for 18 years, permitting rehabilitation of useful vision to the patient in this period. To improve visual acuity in advanced cases, avoiding or postponing a penetrating keratoplasty, several techniques have been described, such as lamellar crescentic wedge resection, exemplified in this case report. Current options in the management of pellucid marginal degeneration. 4 4 Moshirfar M, Edmonds JN, Behunin NL, Christiansen SM. The treatment for PMD is difficult and challenging, due to poor results in visual acuity improvement with glasses, decreasing stability of contact lenses as the disease progresses and the need of a larger and inferiorly decentered graft, closer to the limbus, if penetrating keratoplasty is chosen, increasing the risk of corneal graft rejection. Pellucid corneal marginal degeneration: A review. , 3 3 Jinabhai A, Radhakrishnan H, O'Donnell C.
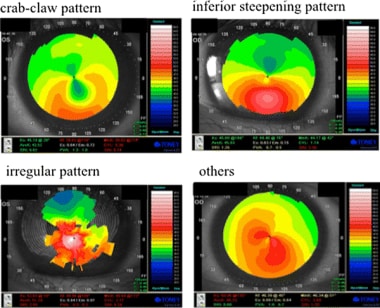
Degeneração marginal pelúcida da córnea: diagnóstico e tratamento. Philadelphia: Elsevier 2005 The gold standard diagnostic test for PMD detection is corneal topography, that will demonstrate flattening of the vertical meridian and higher curvature inferiorly, generating an “against-the-rule” astigmatism, with a “butterfly” or a “crab claw-like” appearance. 1 1 Krachmer JH, Mannis M, Holland E, editors. Pellucid marginal degeneration (PMD) is a bilateral cause of corneal ectasia and is characterized by inferior corneal thinning, approximately 1 - 2 mm in vertical length, typically between the 4 o’clock and 8 o’clock positions, crescent-shaped, with the point of steepest corneal protrusion occurring above the area of stromal thinning.


 0 kommentar(er)
0 kommentar(er)
